People across Plymouth and the wider Devon locality will benefit from more joined-up health and social care from today, 1 July 2021.
Livewell Southwest and University Hospitals Plymouth NHS Trust (UHP) have formally come together as Plymouth’s Integrated Care Partnership. They will be responsible for the delivery of community health, adult social care, mental and learning disability services for adults and older people in Plymouth and the western locality of Devon.
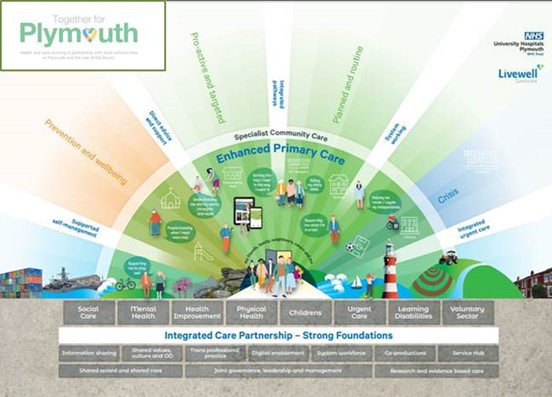
The aim of the partnership is to bring health and social care providers together to create a place-based model of care for Plymouth and the area and build on the work that has already taken place to integrate health and social care. Health and care providers will work to understand and meet the health and care needs of the local population and then design care so the individual citizen is at the centre of a personalised approach.
By working together, UHP, LSW and others, including GPs and the voluntary sector, can build care around the person, supporting them to receive appropriate treatment in the setting that best suits them. This is frequently as close to home as possible.
Integrated care will support those who require care from multiple organisations, whether that is the hospital, community services or a GP. It will also ensure those who are frail, vulnerable or have complex health needs have their care managed more seamlessly. The Partnership will help reduce health inequalities and ensure fair and equitable access and outcomes by supporting preventative health.
After taking feedback from dozens of local people and organisations, the Partnership is committing to people that it will work with them to:
- Build care around you, supporting you to receive appropriate care and treatment in the setting that best suits you. We know this is frequently as close to home as possible.
- Be proactive in planning your care, enabling you to lead a healthy, independent life for longer, with care closer to your home and your community meaning you only have to come into hospital when it’s essential
- Ensure you only have to tell your story once, with health and care professional joining up records
- Empower you to take care into your hands, giving you the tools you need to look after your health and wellbeing
The Integrated Care Partnership is part of a longer journey towards integrated care, which began in 2014 with a vision set out by the Plymouth Health and Wellbeing Board. It also builds on the way partners have come together to respond to the COVID pandemic. For example, the large vaccination centres at Home Park and Derriford Hospital’s Centre for Wellbeing have been jointly run. Staff from UHP, LSW, NHS Devon, Plymouth City Council and the voluntary sector have worked together to engage with people to encourage them to take up the COVID-19 vaccine. This is just one of many examples of closer working. The Partnership will continue to work collaboratively with primary care, the voluntary sector and communities and patients and carers to develop and improve services.
Commissioners identified UHP as the preferred provider, with LSW as a sub-contractor, for the 10-year contract. The start of July will also see the direct management of some community hospital services – community rehabilitation and stroke inpatient beds at Mount Gould Hospital, Tavistock Hospital and South Hams Hospital – transfer from LSW to UHP.
In its first year, the Partnership will focus on seven priorities, all aimed at improving the experience of patients:
- Establishing a Service Hub as the single front door for all services
- Enhanced primary care
- Bringing together care for those people who are most frail
- Delivery of community mental health in line with the framework which will include implementation of a rehabilitation/recovery specialist and dedicated team; implementation of a personality disorder specialist dedicated team; an all-age mental health home treatment offer in place
- Development of end-to-end services for people needing respiratory, cardiology and stroke care
- Further develop and embed a system-based approach to Infection Prevention and Control which can give assurance that standards are consistently high and applied everywhere
- Establish an improved and inclusive mental health model for emergency care
What does integrated care mean for people receiving care – Sally’s story
Sally is a typical fictional patient. Her story demonstrates how things currently work and how they could look under a successful partnership arrangement with organisations working together to meet Sally’ needs and wishes.
Sally’s Story – now
- Sally has lived in the same house independently for the whole of her married life, local friends/family – now a widow
- She has Type 2 Diabetes, high blood pressure, arthritis and is slightly forgetful
- She has fallen a few times – Sally’s daughter sent Sally to hospital, she came home quickly but developed a urinary tract infection and was readmitted
- Sally’s daughter stayed and helped but it took a long time to get help/appointments with geriatrician. She fell again and fractured her hip
- It took Sally a long time to see medical specialists and therapists. She was in hospital for weeks and deteriorated in terms of her own ability to function, for example she went from being able to feed and wash herself to having help with feeding and washing. She kept telling everyone the same story, she was lonely, upset and felt a loss of independence. Sally just wanted to go home
- Eventually – it was decided Sally needed to go to a nursing home and that’s where she is today
Sally’s Story – future
- Sally has lived in the same house independently for the whole of her married life with local friends/family. She is now a widow
- She has Type 2 Diabetes, high blood pressure, arthritis and is slightly forgetful – She has been identified by the primary care team and linked into a named community coordinator, linked to the local GP practice and Health and Wellbeing Hub to coordinate care and undertake a holistic assessment
- The Multi-Disciplinary Team reviewed and linked in with the specialist older people’s team who developed a care plan with Sally and her daughter to enable early intervention to be given and crisis avoided
- Proactive medication review undertaken
- Short-term domiciliary care was arranged to support Sally, then she was transferred to a neighbourhood voluntary scheme run by Age UK
- Sally did fall but a Comprehensive Geriatric Assessment, undertaken on admission to hospital by community and acute staff working together, enabled coordination of future care needs and a Home First approach was taken as was Sally’s wish (What matters to you? compared to What’s the matter with you). The careful assessment and plans put in place helped Sally avoid fracturing her hip.
- Sally remains at home with an anticipatory care plan, support from Age UK and has regular contact with her community coordinator